Disturbances to the circadian clock, which generates the daily rhythms of humans and other organisms, can cause mental stress. Patrick Truss spoke to Dr Gabriella Lundkvist of Karolinska Institutet about her research into the cellular mechanisms of the circadian clock and how they may be altered in psychiatric disease.
The daily rhythms of humans and other organisms are generated by the circadian clock, the internal ‘body clock’, which responds to both genetic and environmental stimuli.
Disturbing these rhythms can lead to mental stress and even disease, an area which forms the primary focus of Dr Gabriella Lundkvist’s research. “The overall objective of my project is to study the cellular mechanisms of the circadian clock, and to investigate if these mechanisms are altered or changed in disease conditions, for instance psychiatric
diseases. These include bi-polar disorder, depression and schizophrenia; we use both human cells and a trans-genic mice model with a luciferase reporter in this work,” she explains. Studies have shown that bipolar disorder and major depression is characterised by rhythm and sleep disturbances; however, it is not yet known if the molecular rhythms of the circadian clock are changed during the disease.
“So-called ‘clock genes’ can be found in most cells in the body, so we can use skin cells from patients suffering from psychiatric disorders to study these molecular rhythms in the cells,” continues Dr Lundkvist. “We take skin biopsies, culture the cells in the laboratory and then study the expression of molecular rhythms in these cultures.”
Seemingly small changes to the molecular clock, such as in its amplitude, can have significant effects on human and animal behaviour. The point is well illustrated by a recent study which showed differences in the period – the time to complete a cycle, effectively a day – of molecular clock cells between the skin of people who prefer mornings and those who prefer evenings. “The difference was not very big – about half an hour – but this has a big impact. If your body thinks the day is half an hour longer then that will result in very big changes after a week in constant conditions,” points out Dr Lundkvist.
Research into the cellular mechanisms of the circadian clock, as well as hormonal rhythms in the blood, holds the key to a deeper understanding of such issues. “The calcium that comes into nerve cells through voltage-gated channels, and also probably intra-cellular calcium, is very important in terms of sustaining and maintaining the molecular clock,” continues Dr Lundkvist. “We think it might actually be a part of the clock itself. The electrical activity of nerve cells affects the molecular clock, so nerve cells electrical signals actually feed back on the genetic expression of clock genes.”
Circadian rhythms
Research suggests calcium is essential to the generation of circadian rhythms; it has been shown in mice and fruit flies that if electrical activity in neurons is stopped then the molecular clock stops completely, while the removal of calcium from a cell culture medium has a similar effect.
However, while calcium is clearly a significant part of the clock machinery, Dr Lundkvist says much remains to be learned about the precise mechanisms behind these processes. “We still don’t know the link between ion channel activity and the molecular clock, which we are currently investigating,” she stresses. This work is made even more complex by the distributed nature of the molecular clock. “There is a centre in the brain, located in the hypothalamus, called the suprachiasmatic nucleus (SCN). These small nuclei appear to co-ordinate and also, in some way, drive clocks in other parts of the body,” explains Dr Lundkvist.
“The liver clock is very important to synchronising rhythms for example. We don’t know how the peripheral clocks feed back into the brain, but it is established that the master clock is situated in the brain, and if we remove this master clock then the individual becomes completely a-rhythmic.” These changes can become marked in older people, as the way the circadian clock functions changes with age. While clock material is present in the body from birth, new-born babies typically follow their mothers rhythms in their early weeks, before developing their own rhythms, which continue to evolve throughout the typical life-span. “Sleep patterns change dramatically as people grow older. We know that sleep patterns become more fragmented as people get older, and you become more sensitive to jet-lag with age,” says Dr Lundkvist.
These changes can cause stress to the body, with potentially serious consequences. “Sleep disturbance can even trigger the onset or relapses of bi-polar disorder, and it is well known that if you sleep too little, have bad quality sleep, or your rhythm patterns are disturbed, then that can lead to depression and contribute to the pathology,” explains Dr Lundkvist. “It has been shown that if patients are kept on a strict regime, and their daily rhythms are controlled with light and food, then they sleep better, which mitigates the effects of the disease. Restoring rhythms can help improve the outcome of treatment; it can accelerate the effects of treatment, and also improve patients’ quality of life.”
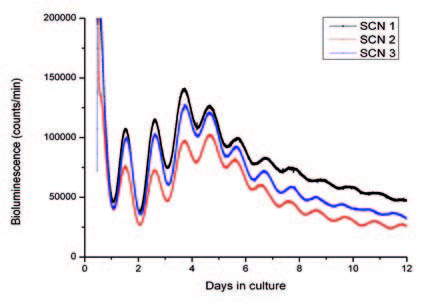
The pacemaker is located in the “suprachiasmatic nucleus” in hypothalamus. The molecular circadian clock activity in the suprachiasmatic nucleus is in the figure visualised using dynamic luciferase reporter technology. The figure shows raw data of luciferase activity monitored as bioluminescence (photon emission), which corresponds to the daily expression of the PERIOD 2 protein, one of the key players in the molecular clock. Three organotypic tissues (represented by black, red and blue) containing the suprachiasmatic nucleus from transgenic mice held in a 12 light:12 hr dark cycle were cultured for 12 days. The PERIOD 2 protein expression is typically high at the onset of subjective darkness and low at onset of subjective day.
Treating depression
Sleep disturbance is of course just one aspect of depression and psychiatric disorders, and can be both symptom and cause, but it is nevertheless an important focus for treatment. One of the key issues Dr Lundkvist is addressing, that of whether the circadian clock is equally robust and stable in somebody suffering from depression as it is in a healthy person, holds real relevance in this regard. “Our working hypothesis is that the clock isn’t as robust in sufferers of bi-polar and uni-polar depression. For instance, if the oscillations of the clock have a lower amplitude, as has been suggested in a recent study, it could weaken the clock; we think that could make the clock more sensitive to environmental stimuli,” she outlines. Preliminary data suggests that calcium signalling in the cells of patients with bi-polar disorder and schizophrenia is weaker than in healthy people, but Dr Lundkvist is wary of drawing swift conclusions. “These differences in calcium signalling would hypothetically affect the molecular clock, but they would also affect many other processes as well,” she cautions. “Depression can’t be understood in terms just of changes to the molecular clock, it’s not that simple. But the circadian clock is a very old feature of all organisms and it evolved very early in the life of earth, it seems to be essential to all cellular processes.”
This is reflected by the number of other conditions in which the circadian clock plays a role. It has been shown that certain types of breast cancer are associated with shift work, while sleep disturbance is also a key characteristic of certain neurodegenerative diseases, demonstrating the wider relevance of Dr Lundkvist’s work.
“Parkinson’s disease and Alzheimer’s disease are both characterised by sleep disturbances, and also in some cases by depression. We think that these sleep disturbances might be related to the aging process of the brain,” she says. No firm conclusions can yet be drawn from the data in terms of how calcium levels affect clock function, but Dr Lundkvist has preliminary results showing that some commonly used psychotropic drugs can act as chronobiological substances and help set the time of the circadian clock, and hence form a key part of treatment. “Some people may need assistance in re-setting or ‘boosting’ circadian rhythms, and certain medicines can stabilise the circadian clock,” she continues. “We know a lot about lithium for example and how it appears to stabilize the circadian clock, information which is very important to the people who take it.”
Much of this research has been undertaken on mice, from which tissue or cells are extracted and cultured in organotypic and primary cultures. However, Dr Lundkvist also has access to material from patients at the Karolinska Institutet University Hospital.
“I work with a small group of clinicians, including Professor Jerker Hetta and Dr Björn Owe-Larsson, who provide us with patient material which we take directly to the laboratory and use for molecular studies, which is unique. From there we can look at the medications currently used in hospitals and how they can be improved,” she says. While this is of course enormously important research, Dr Lundkvist says her future agenda balances both fundamental and applied work.
“Fundamental research is the foundation of the great scientific findings, it’s extremely important,” she stresses. “There’s so much to learn about so many aspects of both the brain and the circadian clock. There are big gaps in our knowledge of the key mechanisms; we don’t know about the link between calcium and the molecular clock for instance – that’s something we need to address before we can go on and use our knowledge in clinics.”



 Download this article as PDF
Download this article as PDF


